Medical Gaslighting: How To Spot It Before It Hurts You?
2 months ago
5 minute read.

Have you ever walked out of a doctor’s office feeling dismissed, unheard, or even doubting your own body? You know something is wrong, yet the professional you trusted seems to brush it off. If this sounds familiar, you may have experienced medical gaslighting.
Medical gaslighting happens when healthcare providers minimize, downplay, or outright ignore your symptoms, often making you feel like the problem is “all in your head.” It’s a subtle but damaging form of invalidation that can delay diagnosis, worsen health conditions, and take a toll on your mental well-being.
Unfortunately, many people—especially women, young adults, people in larger bodies, and those with chronic illnesses—have faced some form of medical gaslighting. Recognizing the signs is the first step toward protecting your health and getting the care you deserve.
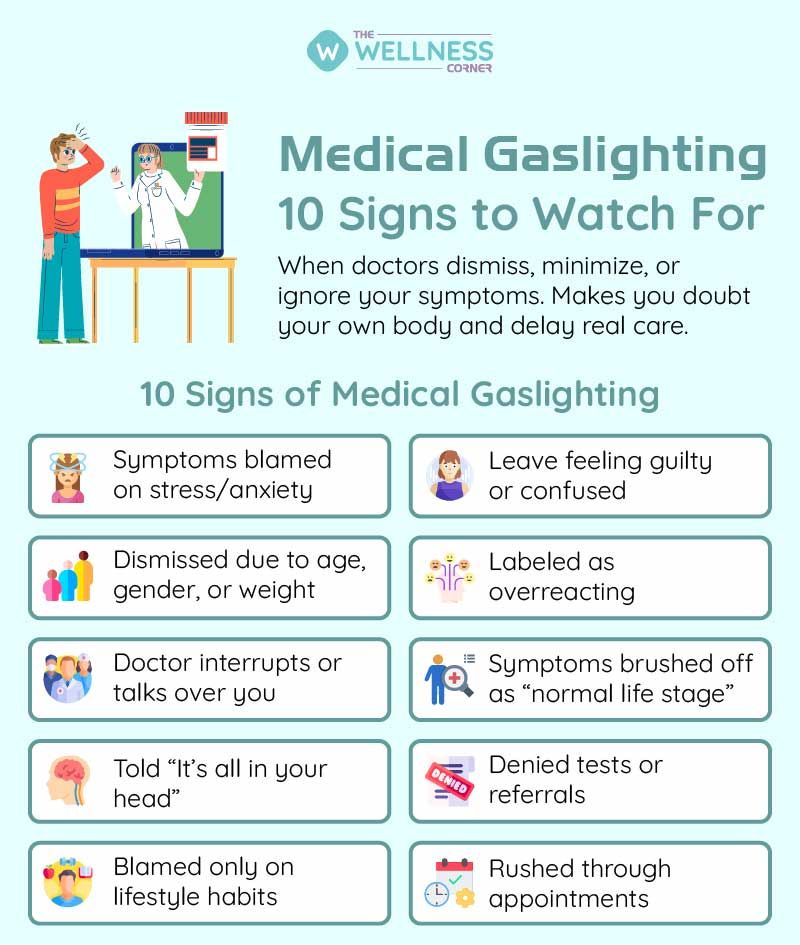
Here are 10 signs of medical gaslighting to watch for, with real-world examples you might relate to:
1. Your Symptoms Are Dismissed as Stress or Anxiety
It’s normal for doctors to consider stress as a factor, but it should never be the only explanation given without proper testing. For example, someone complaining of ongoing fatigue and palpitations might be told, “You’re just anxious, try to relax.” Later, they may find out they actually had a thyroid disorder or heart issue.
What to do: If you hear this repeatedly without testing, ask: “What tests can we run to rule out other causes?”
2. You’re Not Taken Seriously Because of Your Age, Gender, or Weight
Bias in medicine is very real. Young people are often told they’re “too young to have anything serious.” Women’s pain is often minimized compared to men’s. And people in larger bodies frequently hear, “Just lose weight,” even when their symptoms have little to do with weight.
Example: A 28-year-old woman with severe stomach pain might be told it’s “just period cramps,” only to later discover she has endometriosis.
What to do: Remind your provider that age, gender, or weight don’t rule out illness and request further evaluation.
3. The Doctor Interrupts or Talks Over You
If your doctor keeps cutting you off or seems impatient, that’s a sign they’re not truly listening. Imagine going in to explain weeks of migraines, but the doctor interrupts with: “It’s probably just screen time—take some painkillers.” You leave feeling like your experience didn’t matter.
What to do: Bring written notes of your symptoms and insist on finishing. If they don’t allow space, it may be time to find a new provider.
4. You’re Told “It’s All in Your Head”
This phrase is the hallmark of gaslighting. Many people with conditions like fibromyalgia, autoimmune disorders, or chronic fatigue syndrome were once told they were “imagining it.” Years later, their condition was validated by research.
Example: Someone struggling with widespread body pain might hear, “There’s nothing wrong with you,” leaving them to doubt themselves.
What to do: Trust your instincts—your lived experience is real. If dismissed, seek a second opinion.
5. Your Symptoms Are Attributed Only to Lifestyle
Lifestyle choices do affect health, but not everything is explained away by diet, exercise, or sleep. If you complain of persistent bloating and fatigue, being told “drink more water and sleep better” isn’t enough.
What to do: Acknowledge lifestyle factors but press for medical testing: “I’ve already made changes, but the symptoms continue. What else could it be?”
6. You Feel Rushed Through Appointments
If your doctor spends only five minutes with you and hands you a prescription without hearing the full story, that’s a red flag. Many patients leave such visits feeling more confused than when they entered.
What to do: Prepare your top 2–3 concerns in advance so you’re not brushed aside. If the rushed approach continues, consider switching providers.
7. You’re Denied Tests or Referrals
Sometimes patients request specific tests because they sense something is wrong. But if the doctor refuses with: “That’s unnecessary” or “You’re overreacting,” without explanation, it may prevent early diagnosis.
Example: A patient repeatedly asking for a cardiac test is denied, only to suffer a heart attack later.
What to do: Ask, “Can you explain why this test isn’t necessary?” A transparent doctor should provide a clear reason.
8. Your Condition Is Blamed on Normal Life Stages
Life stages like puberty, pregnancy, menopause, or aging can cause changes—but they should not be a blanket explanation for everything. A 55-year-old man with chest pain being told, “It’s just aging,” or a woman with heavy bleeding being told, “It’s just menopause,” are examples of harmful dismissal.
What to do: Ask, “If this is normal, why does it feel different from before?” This helps open discussion about other possible causes.
9. Your Concerns Are Labeled as Overreacting
If you’re told “you’re exaggerating” or “it’s not that bad,” your pain is being minimized. Pain thresholds vary, and even “mild” symptoms can point to serious conditions.
Example: A child repeatedly complaining of knee pain may be brushed off as “growing pains,” but it could be juvenile arthritis.
What to do: Keep a log of your symptoms to show patterns—this makes it harder to dismiss.
10. You Leave Feeling Confused or Guilty
The biggest red flag? Leaving an appointment feeling like youdid something wrong. You may feel guilty for “wasting the doctor’s time” or question whether your symptoms are real. That’s gaslighting at work—it shifts blame to you instead of addressing the issue.
What to do: A supportive doctor should leave you feeling informed, not confused or guilty. If that’s not the case, it may be time to seek support and stand up for yourself in a different space.
How to Protect Yourself from Medical Gaslighting?
Spotting gaslighting is just the first step—taking action is what truly protects you. Here are some practical ways to safeguard your well-being:
- Listen to your gut — when something doesn’t feel right, pay attention to it.
- Bring notes – Write down your symptoms, including when they started and how often they occur.
- Ask questions – Don’t hesitate to ask, “What else could this be?” or “What tests can rule out other causes?”
- Seek a second opinion – Another doctor may offer a different perspective.
- Bring support – A friend or family member can validate your concerns in the room.
- Keep records – Track medical visits, prescriptions, and test results.
Final Thoughts
Medical gaslighting can leave patients feeling powerless, but awareness is the first step toward change. If you’ve ever been dismissed, told “it’s all in your head,” or left doubting your own body, know this: your experience is valid.
The healthcare system should be built on listening, respect, and collaboration. You have the right to be listened to, respected, and cared for properly. If your provider isn’t doing that, it’s okay—and necessary—to advocate for yourself and seek someone who will.
Your health is too important to be brushed aside.
Leave a Comment
Related Articles
Health Checks @ Home
Service
Explore
© 2025 Truworth Health Technologies Pvt. Ltd.




